- Valve-in-valve (ViV) TAVI has been shown to be a viable alternative to redo (reoperative) surgery in patients with degenerated surgical (sAVR) or TAVI bioprosthetic valves1
- Patients with severe aortic stenosis (sAS) presenting with a change in clinical symptoms should be referred to the Heart Team for ViV TAVI evaluation
- Evidence suggests ViV TAVI provides favourable clinical outcomes for patients2
More patients are having TAVI, earlier in the pathway
Increasingly sAS is being diagnosed earlier, with more people receiving valve replacement at a younger age.3
Most bioprosthetic valves are free from deterioration for up to 15 years and — although many patients have an increased life expectancy due to the initial valve intervention — the valve may need to be replaced at some point.4
ViV TAVI has been shown to be a viable alternative to reoperation in patients with a degenerated sAVR or TAVI valve.1
In their 2020 consensus paper, DGK/DGTHG recommends ViV TAVI for patients with a failing bioprosthetic valve.5
Identifying the right patients for ViV TAVI
Redo surgery has conventionally been the standard of care for patients with a failing bioprosthetic valve. The morbidity and mortality associated with reoperation is significant, however, many patients are refused for redo surgery.3
The latest clinical evidence suggests ViV TAVI can offer favourable outcomes in patients with a failing bioprosthetic valve.2
Review the data recommending all patients with a failing valve should be referred to the Heart Team for TAVI evaluation.
Review the dataCarrying out ViV TAVI
Patients presenting with a change in clinical symptoms should be referred for tests to confirm if the initial bioprosthetic valve is failing and therefore requires replacement.
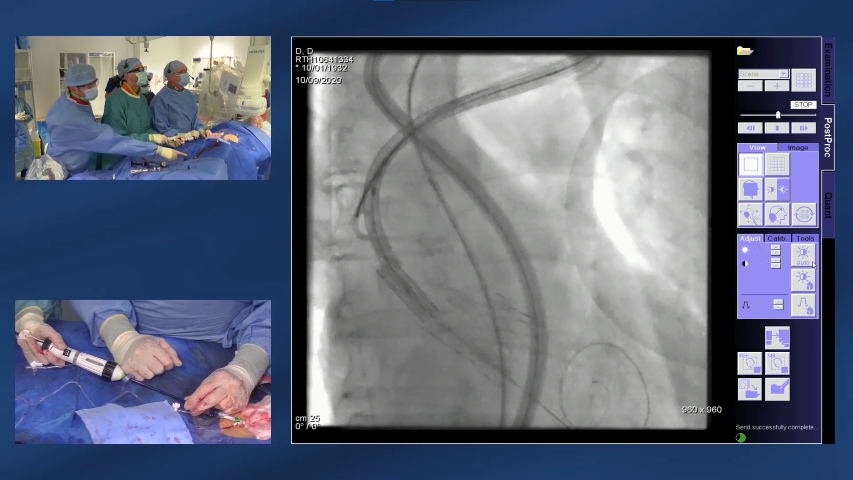
- The ViV TAVI procedure is similar to an initial TAVI intervention, with the failing valve used to guide the positioning of the replacement valve6
- The replacement valve is gradually deployed and the new bioprosthetic valve is placed tightly into the inside of the failed valve, pushing the old valve leaflets aside6
- Angiography is used to ensure accurate positioning of the valve6
Improved clinical outcomes from ViV TAVI
ViV TAVI is associated with lower early mortality and morbidity, and increased survival at a follow up of 5 years, compared with redo surgery.1
Clinical and registry data show favourable early outcomes in patients treated with ViV TAVI1

Real-world data show high risk patients treated with ViV TAVI showed favourable outcomes2


Reducing health system impact
ViV TAVI can minimise the patient’s hospital footprint by lowering rates of resource-heavy complications. Comparative studies show that ViV TAVI is associated with shorter stays in the intensive care unit (ICU), reduced time on ventilation and lower transfusion requirements compared with redo surgery.7
Real-world data demonstrate that ViV TAVI resulted in low patient exposure to the healthcare system.2
Results:
- 44.5% experienced conscious sedation
- 22 hours spent in ICU (median)
- 2 days spent in hospital (median)
References:
1 Tam DY, et al. JACC Cardiovasc Interv. 2020;13(6):765—774.
2 Kaneko T et al. Valve-in-Surgical Valve with SAPIEN 3 for Transcatheter Aortic Valve Replacement: Propensity-Matched Analyses of Real World Data Based on the STS Predicted Risk of Mortality. Presented at TVT Connect. June 20, 2020.
3 Rodriquez-Gabella T, et al. J Am Coll Cardiol. 2017;70(8):1013—1028.
4 Paradis J-M, et al. J Am Coll Cardiol. 2015:66(18):2019—2037.
5 Kuck K, et al. Cardiologist 2020;14:182—204.
6 National Institute for Health and Care Excellence (NICE). IPG653. Available at: https://www.nice.org.uk/guidance/ipg653/chapter/2-The-condition-current-treatments-and-procedure (accessed March 2021).
7 Silaschi M, et al. Interactive CardioVascular and Thoracic Surgery. 2017:24(1)63—70.
Medical device for professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
PP--EU-1713 v2.0